T cell receptor (TCR) engineered T-cell therapy shows tremendous potential in combating metastatic melanoma, synovial sarcoma and myeloma, as evidenced by numerous ongoing clinical trials. Despite this promise, identifying the appropriate T-cell receptors (TCRs) with desired functionality has proven challenging, leading to a lack of clinically approved TCR-T cell therapies thus far.
Overcoming limitations of conventional in vitro assays to identify efficacious TCRs
Optimal TCR selection requires thorough preclinical characterization using an array of in vitro assays to gain critical insights on molecular kinetics and functional outcomes. However, these methods have multiple limitations and often fail to adequately identify the most optimal TCR for therapy.
Affinity: Readouts on molecular kinetics and affinity of TCR binding often disregard the interactions of multiple TCR-pMHC complexes and co-receptors, resulting in poor correlation to TCR functionality (Zhang et al., 2018).
Peptide Titration: T-cells are stimulated with peptides and sorted based on activation markers, yet the potency of identified TCRs is often poor (Mateyka et al., 2022).
Cytotoxicity: While providing critical data on the functional outcome, this assay requires appropriate target cell lines with the correct HLA restriction and target antigen to achieve reliable and accurate results (Carr et al., 2024).
pMHC Multimers: Peptide-major histocompatibility complex multimer staining directly measures dissociation kinetics of T cells with the co-receptor but does not offer a comprehensive measurement of cell-cell binding critical for immunological synapse initiation (Nauerth et al. 2016).
The outlined limitations of conventional assays for identifying functional TCRs can impose substantial time and financial burdens on immunotherapy development when suboptimal candidates are selected. Optimal TCR selection for cell therapies necessitates thorough preclinical characterization, prompting Carr et al., to focus on comprehensive cell-cell binding assessment, termed Cell Avidity. Unlike traditional methods, cell avidity takes into account all cellular interactions that take place during the initiation of an immune synapse. This novel measurement bridges the gap between molecular kinetics and functional outcomes, enhancing preclinical decision-making by evaluating potency, safety, sensitivity, and cellular kinetics. Compared to conventional methods, this approach was demonstrated to improve correlation with functionality, thereby potentially accelerating the development of effective TCR-T therapies.
TUM researchers leveraged Cell Avidity to identify functional TCRs using their flexible Jurkat system
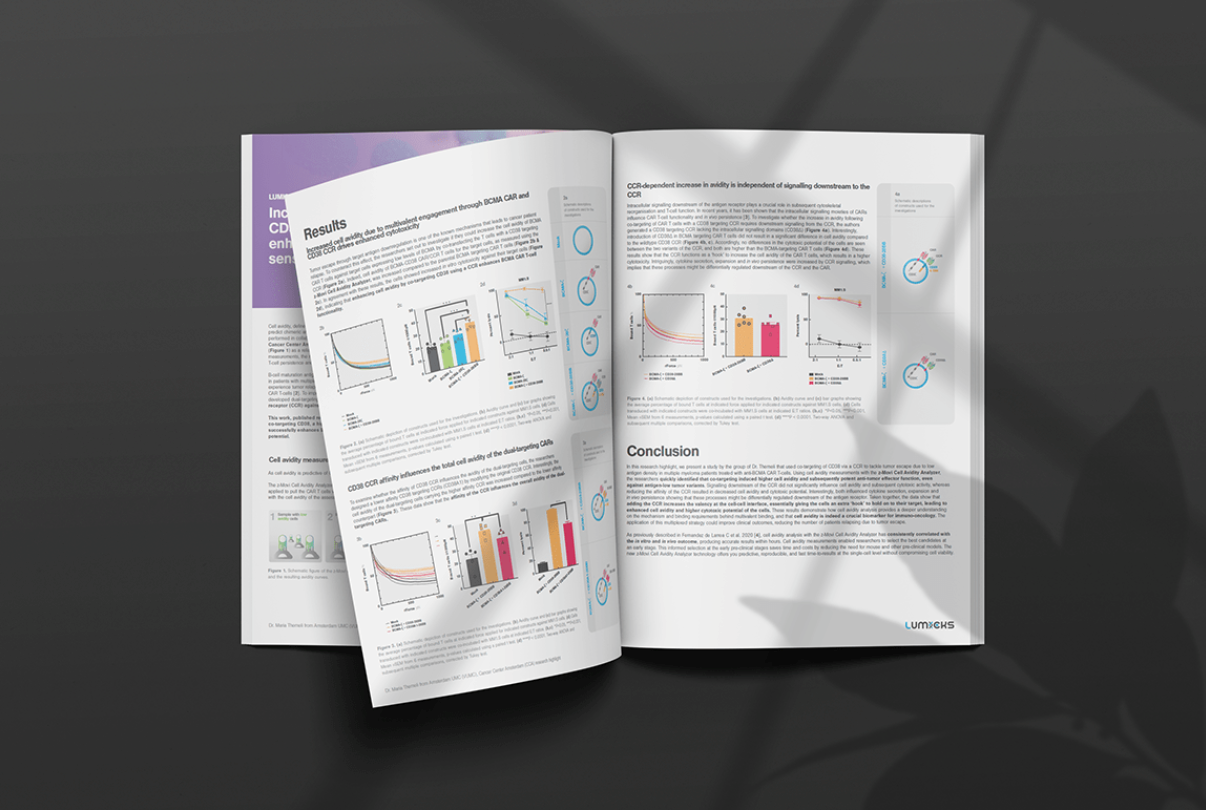
In a recent study published in Biological Chemistry (2024), researchers leveraged Cell Avidity measurements to identify functional TCRs efficiently. Led by Professor Dirk Busch and Dr. Elvira D’Ippolito, the study sought to address the limitations of conventional in vitro techniques by exploring whether full cell-cell binding characterization, by cell avidity, correlated with TCR functionality.
The researchers developed a flexible system for TCR re-expression using a Jurkat triple parameter reporter cell line (J-TPR), a widely used model system in immunology research.
With the platform established, the researchers focused on characterizing cell-cell binding using the z-Movi Cell Avidity Analyzer technology. This advanced assay measures the binding probability between T cells and tumor cells, providing accelerated processing and strong correlations with T-cell functions. Cell avidity measurements reliably identified high- and low-functional TCR-T cells for both RNF43- and SARS-CoV-2 specific TCRs (Figure 1A). Intriguingly, among the panel of RNF43-specific TCRs, TCR-32 demonstrated the highest peptide sensitivity (Figure 1B); however, it ranked the third lowest in total NFAT activation (Figure 1C). Although the responsive cells showed high sensitivity to peptide stimulation, they made up only a small fraction (20%) of the TCR-expressing cell population. This highlights that the majority of cells carrying the TCR did not engage in productive TCR signaling (Carr et al., 2024). This suboptimal phenotype was identified using cell avidity (ranking third lowest of bound J-TPR cells), whereas the peptide sensitivity assay did not detect the poor functionality.
These findings underscore the potential of cell avidity as a reliable parameter for identifying intricate phenotypic behavior impacting TCR function. By integrating cell avidity measurements with their versatile T cell engineering platform, the researchers established a model system for enhancing their decision-making during the in vitro selection process of functional TCRs.

How does complete cell binding characterization enhance the selection of functional TCRs?
The current landscape of TCR-T cell therapies has made significant progress, highlighting their clinical effectiveness across a range of tumor targets. Although no TCR-T cell therapies have received FDA approval, Tebentafusp, a TCR/anti-CD3 bispecific targeting HLA-A02:01-gp100 and CD3, was approved in early 2022 for metastatic uveal melanoma, showing a significant survival rate improvement in a phase 3 trial. Moreover, Afami-cel from Adaptimmune is a leading TCR-T cell therapy targeting HLA-A02:01-MAGE-A4 showing encouraging clinical results in a phase 2 trial leading to a Biological License Application (BLA) fast-track by the FDA. However, despite these advancements, toxicity remains a concern. TCRs can sometimes exhibit promiscuous recognition of unrelated epitopes from normal proteins, leading to off-target toxicity, as seen in the MAGE-A3 TCR clinical trial (Linette et al., 2013).
The field continues to rely on a protracted preclinical selection process, which utilizes conventional assays like affinity, cytotoxicity and peptide titrations that often correlate poorly with T-cell functionality and fail to identify toxicity problems. Integrating cell avidity into the TCR selection process offers researchers a comprehensive toolbox to fully characterize cell-cell binding to target antigens, addressing potency, safety, sensitivity, and cellular kinetics. This enhances decision-making carried out in vitro to select TCRs with higher likelihoods of functionality in vivo. Such integration is essential for improving the efficacy and safety of emerging T-cell therapies, thereby advancing the field towards more precise and effective therapeutic interventions.